Here I am, long overdue for an update yet again. So how are things going over here? Well, iIf my five year old daughter, Ryan, could sum it up for you, she’d likely throw her little fingers up into the most confident air quotes you’ve ever seen and say “Mommy’s head has felt soooo good these last seven months.” She’s still working through the nuances of sarcasm and irony but in this particular instance, well….she ain’t wrong.
The truth is, these last 6 months (9 months…12 months) have been filled with some of the worst pain days of the last 13 years. And given what the last decade + has been like, that’s a real gut punch just to type. For no identifiable reason, my headache has been so terrifyingly out of control. I can’t even think of another way to say it. It’s also been a very challenging few months working through one insurance denial after another, which I’ll get into.
In my last post last March, I recapped my trip to Park City to see Dr. Kutcher, the neurologist I’d been working with for the past 2.5 years. When I returned home to Arizona, I continued working remotely with his vestibular physical therapist, but the vestibular rehab was wrecking absolute havoc on my headache. That could be a positive indication that those systems are in play, but by the end of spring we had all decided it needed to take a backseat just so I could regain baseline function.
I’ve responded similarly to vestibular work in the past so it wasn’t entirely surprising, but incredibly frustrating nonetheless; to be working so hard just to gain an inch of traction and instead slipping, slipping, slipping further into pain that feels so inescapable.
Here are a few snapshots of pain flares in action. These skin changes on my neck are indicative of of the CRPS that gets triggered during some (but not all) of my worst increases in head pain. Cute, right?
By the end of March, I had completely stopped ketamine. We had a few new medications to try though - just anything to make even the smallest dent in my headache would be a win. Though I typically don’t have adverse reactions to most that I try, a few of these didn’t end well for me. First up was an anti-seizure drug called Lamictal, which is one of those meds you start at a low dose and gradually ramp up. That didn’t help and actually gave me hives (not the best, not the worst). Side note: If you're new here, I don't have (and never have had) seizures but these kind of anticonvulsants are often used to treat chronic pain because they help regulate abnormal electrical activity in the nervous system, which is also implicated in neuropathic pain, where damaged nerves send excessive pain signals to the brain.
There were two more antiepileptics. The first was Keppra, which provided nothing aside from a whole lot of fatigue and then, Oxcarbazepine. Oh, Oxcarbazepine. That one caused quite a bit of nausea and by the end of week one, I was headed straight from the parking lot of Ryan’s Sunday morning soccer practice to the emergency room. I’ve never thrown up more in my entire life. And that level of throwing up took my head to a level of pain where I was barely conscious. “Fun times” Ryan might tell you.
Mid-spring, I had gotten some Botox (just because it had been quite a few years and felt like it couldn’t hurt to try again) but after the second round a few months later, Dr. Kutcher suspected I could be experiencing a flare due to its wear off. I mean, that doesn’t feel fair.
Through the summer, I tried an abortive analgesic called Fioricet, in combination with Toradol. Many years ago, Dr. Dodick at Mayo would sometimes write me a prescription for Toradol (a non-steroidal anti-inflammatory) that Craig would inject. During super intense pain flares, the Toradol, albeit temporary, would sometimes help take the edge off. Unfortunately, not the case at all this time around.
Then there was Quilipta, an anti-CGRP migraine drug (also known as an CGRP inhibitor or CGRP antagonist). This class of migraine meds that are supposed to treat the pain by blocking the activity of a protein called calcitonin gene-related peptide (CGRP), which is thought to play a significant role in triggering migraine pain by causing inflammation in the membranes surrounding the brain. These medications bind to CGRP or its receptors to effectively prevent the activation of pain pathways. Some are abortive but most are preventative.
It’s sort of wild to reflect on the evolution of migraine medicine in the 13 years I’ve suffered. I remember sitting at Mayo with Dr. Dodick back in 2012 and hearing about these new medications that would be gaining FDA approval in the coming years. And If you’ve been following along for a while, you might recall that I’ve tried several CGRP antagonists before.
Over the past few years, I’ve been on Ajovy, Aimovig, Nurtec, Ubrelvy, and Zavzpret. Obviously none have helped me, but patients can respond very differently to each which is why you can’t write off the entire class of meds based on your experience with just one.
The fatigue I experienced from Quilipta was no joke, especially coupled with my sky high pain levels. I was struggling to make it to Ryan’s 7pm bedtime, crawling into bed myself as soon as she was asleep. It’s one thing to endure an unwanted side effect when a medication IS helping, but it’s really shitty to be experiencing those downsides when the medication isn’t even touching your pain. It feels like being kicked when you’re down and not even having the energy to get back up.
Most recently (just last week), II tried yet another CGRP drug called Vyepti. Vyepti is a once-every-3 months infusion, whereas the others have been either injectable or oral medications. I was able to have Vyepti administered by a nurse here at home, which was at least convenient. IV pole to my right and my Charlie girl curled up at my feet. So far, I haven’t felt any benefit but possibly still too soon to write it off.
The last medication worth mentioning is an Oxytocin nasal spray. There's some interesting research to support oxytocin as a modulator of pain perception and a natural pain reliever due to its analgesic properties and ability to reduce stress and anxiety associated with chronic pain. Oxytocin interacts with pain pathways in the brain, potentially by activating the endogenous opioid system, leading to pain reduction. And the most direct way to deliver oxytocin to the brain is intranasal spray. I've been using this prescription spray for a couple of weeks now. So far I can't say I've felt anything but the dosage is gradually titrated so we'll see if I notice anything. Can't hurt to try.
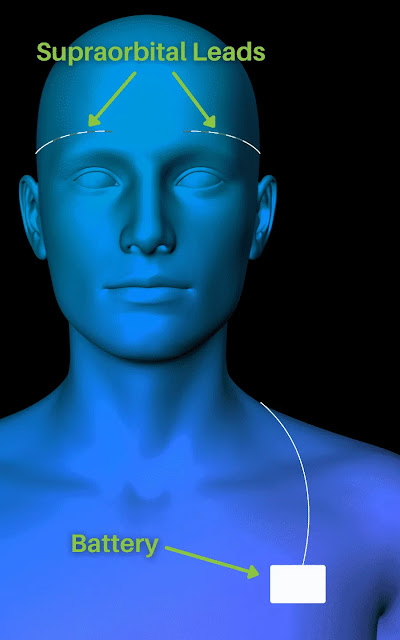
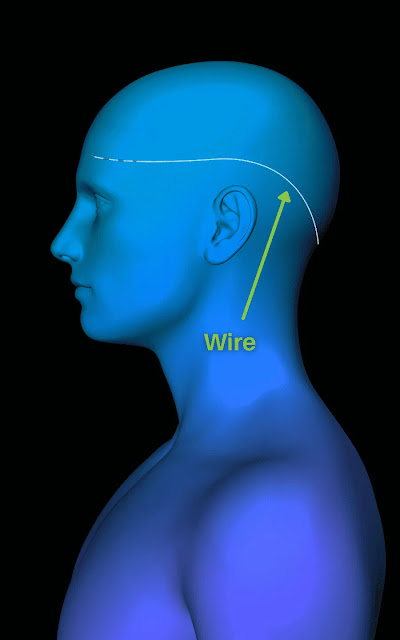
So now rewind for a minute back to April/May. Craig and I met remotely with a new doctor based in Dallas, Dr. Kenneth Reed of US Migraine (now Reed Migraine). Dr. Reed is the inventor of the “Reed Procedure” for migraine treatment. Simply put, the Reed Procedure involves implanting a small device under the skin near the occipital nerve, which delivers mild electrical pulses to disrupt pain signals and alleviate severe chronic migraines in patients who haven’t responded to other treatments (hi, it’s me!). It works by targeting the nerves in the supraorbital and occipital regions of the head (hi, it’s my headache!)
It wasn’t that this procedure has never been on our radar. We actually spoke to Dr. Dodick at about it a decade ago but at that time, implanted neurostimulators for chronic headache involved wire leads running under the skin up along the spine and I was told that it would likely have an effect on my ability to be active.
Craig and I had a really thorough and thoughtful conversation with Dr. Reed. He explained that patients first undergo a temporary TRIAL stimulator first to ensure that the procedure works for them before fully committing to the permanent implant. During the trial, they implant a temporary unit underneath the skin (similar to an IV tube) which stays in for just 3-7 days. I’d stay in Dallas during that time and have it removed before flying back to Arizona. For patients who experience relief with the trial, the effects are typically dramatic, which allows them to make a decision of whether or not to proceed with the permanent stimulator with a good deal of confidence.
For the permanent stimulator procedure (which would be on a separate trip), two leads are superficially implanted right underneath the skin along the supraorbital nerves above each eyebrow.
Two leads are superficially implanted right underneath the skin along the occipital nerves in the back of the head.
And a battery/pulse generator device is superficially implanted right underneath the skin on the left side of the chest.
Even though the leads, battery, and connecting wires are right under the skin, they’re not at all externally visible so you would never know by looking at someone that all this magic is happening just beneath the surface. Honestly though, if it took my pain away, I’d proudly rock that look all day every day.
There was no doubt from Dr. Reed that I’m a prime candidate for the surgery. And from my perspective, it also feels like there’s not a whole lot to lose moving forward with the trial. If it works, life changing. If it doesn’t, I’m not worse off than I am now. Reed Migraine states that the stimulator does work for over 80% of their patients, which is very encouraging. But I’ve also learned not to get too attached to stats and success rates and just take it one step at a time.
Here’s where things got a little bumpy for us. As soon as we had that phone call with Dr. Reed and had all my records sent over, we began the pre-authorization process. Over the course of thirteen years, Craig and I have been through the ringer with insurance. And as you might guess given every treatment/therapy that I’ve pursued, there has been quite a lot that we’ve come out of pocket for. But even the majority of medications and procedures that have been covered have only been approved after initial denials, appeals, more denials, peer-to-peer reviews, etc. And hey, I get that those systems are in place for a reason and I don’t think I’m an exception to the rule. But the shit we’ve been through trying to get treatments approved is absurd. For example, several years ago I was having a nerve block done under CT guidance. The procedure was denied, appealed, and ultimately approved. My pain management doctor opted to perform each side on different days for both safety reasons and to better identify a pain source (so technically they were treated as separate procedures). After the whole rigmarole of getting the first one approved and performed, the second side was denied and we had to restart the whole appeal process. That just paints you a little picture of what we're working with here.
Or take the Yvepti infusion I had just last week. It was submitted to insurance along with 65 pages of my headache treatment history from my neurologist. I received a denial letter saying:

I haven’t had more than 4 migraines per month? How about every day of every month for approximately 160 months and detailed medical records documenting 13 years of treatment? What the actual fuck.
The letter goes on to explain that Yvepti is only considered medically necessary if I’ve tried (without success) the other anti-CGRP drugs and then goes on to list Ajovy, Aimovig, Nurtec, and Ubrelvy. Do you remember a few paragraphs ago when I listed those CGRP medications as ones I've tried in the last 2 years? If so, congratulations - you've already read more than the person whose literal job it is to review my required medical history and determine the fate of my treatment. Back through the appeal process we went and fortunately, Yvepti was ultimately approved.
My intention in rehashing this isn’t to dwell on bullshit I obviously have no control over. I like to think that it’s not in my nature (or Craig’s) to assume the worst of others’ intentions, but it is just mind numbingly insane to me that it is someone’s job to review my records and make a decision on very objective criteria and they can just fail at it so hard. And all at the expense of my pain. I would love nothing more than to stand face to face with an individual who is making these determinations and ask them to consider the human being on the receiving end; to ask them to imagine if that person suffering was their wife, husband, child, or parent.
Anyway, sometimes the appeal process IS fairly straightforward, but in the case of this Reed Procedure, it’s taken approximately 7 frustrating months. Fortunately, Craig is (and always has been) my biggest advocate and he takes this all head on. If you only knew the hours he’s spent on the phone with the insurance company, the case managers, the benefits team, the doctors offices, the attorney, trying to sort it all out. It makes me feel so grateful for him but also infuriated that this is the system people in my position have to fight against. Chronic pain warriors, many of who struggle just to get through the day, have to battle the very insurance companies we are PAYING customers of, just to get the care we need. And sometimes even then, it’s still not enough.
Obviously our goal was to not be paying cash for this surgery. We fought through appeals, the clinic resubmitted under several codes since I technically have more than one diagnosis (including complex regional pain syndrome), and through each step of the process, the insurance company maxed or exceeded their “response window” before sending the rejection. The last step was an external review, which was ultimately denied just a few weeks ago. So that really blows.
The positive is, we are moving forward with the Reed Procedure regardless. And another positive is that we pay up front for both the trial and the permanent implant but if the trial doesn’t work for me, we get a complete refund. That is not even close to common practice, and is one more reason we feel so confident in giving this thing a shot. If it doesn't work, I'll know I've given it a fair shot and if it does work, it'll be the best money we've ever spent and maybe will ever spend in our lives. Cautiously optimistic as ever.
My trial is scheduled for early January. So Craig, Ryan, and I will head to Dallas for about 5 days. I'll get all wired up on a Tuesday morning and sort of go about the next few days as normal. For patients that have identifiable triggers, they're advised to lean in to all the things that spike their pain with the temporary stimulator. For me, that shouldn't be an issue. Then it'll be removed on Friday and FINGERS CROSSED, I'll be elated with the outcome and the surgery can be scheduled not long after.
I'll update more from Dallas!