Hello friends and strangers. It's been a while, as it always is. But thank you for checking back in, or perhaps landing here for the first time, in your own fight for freedom from chronic head pain. I know these last twelve months have rocked pretty much everyone's worlds in all kinds of unprecedented, unfathomable ways. And if you live with chronic and unrelenting pain, the hill you climb every day is still the hill you climb every day. I'm sure many of you have spent this year climbing it with fewer resources, less treatment, less support, less hope. So even if the answer to your (our) pain still doesn't feel within reach, here's to hoping that it can finally start to feel just a little more possible.
I figured I'd go through some updates, bullet point style. Spoken like a real, time-starved and just a little bit exhausted toddler mom, am I right? These are in (mostly) chronological order since early December.
- Stem cells: The February update from Regenexx Grand Cayman is that the island is continuing with a cautious, phased reopening of their borders. The next stage is contingent on first having 90% of persons over the age of 60 vaccinated. Once that objective is achieved and borders are reopened, Dr. Centeno's office will be able to reopen (hopefully later in the year). So, my stem cells are still there, safely sitting in cryopreservation storage. Though I prefer to envision them lounging in the warm sand with little umbrella drinks, waiting patiently for me.
- Z Health: I had mentioned before that I was starting some "neurocentric" rehabilitation with a Z-Health practitioner. After my initial evaluation, I was prescribed a series of vestibular exercises (along with some specific breath work). VOR, or vestibular ocular reflex (think gaze stabilization) is used to retain the eyes, inner ear, and brain to work together after head injuries. I think there's certainly a lot of value in this approach, and I stuck to my daily rehab for about a month or so but honestly wasn't experiencing any change in symptoms.
- Postoperative pain flare: In early December, I had a septoplasty to correct a deviated septum from an old soccer injury. When I was sixteen, I headed an opponent's head instead of the ball (oops) and quickly watched my beautiful cleats turn from white to red. I drove myself to the ER and cried every time I looked in the rearview mirror because of how crooked my nose looked. Hah! It only needed a surgical manual realignment at the time, but my nasal breathing has never totally recovered. Not a huge deal, but over the years, as I've tried different breathing techniques to help manage my head pain, my compromised nasal passageways had become more glaring.
If you're not familiar with the benefits, nasal breathing has a few advantages over mouth breathing. Essentially, it allows for more oxygen to get to active tissues, as nasal breathing releases nitric oxide. Nitric oxide is needed to increase CO2 in the blood, which is what releases oxygen. So when you're constantly breathing through your mouth, your body's cells simply aren't getting as much oxygen. And when your body is under a constant state of stress (hi, chronic pain!), you're really just making a tough situation worse. So, I figure now was as good a time as any to have my deviated septum corrected. I may not take things as far as my freak-of-nature husband and go for mountain bike rides or perform versa climber sprints with my mouth closed, but at least I can breathe more easily.
The reason I'm even bothering to bring this up is that I experienced an incredibly severe head pain response to surgery. I felt fine immediately after (as in, normal-high headache) but as the night went on, it began to spike, reaching a really out of control, truly scary level of pain. This seems to be a pattern when my body is undergoing any kind of additional trauma. It happened during my Topomax-induced kidney stone "vacation" to Mass General in 2015 and during my unmedicated labor with Ryan (and to a slightly lesser degree, during a bout with mastitis during my early days of breastfeeding). Unfortunately, pain at this level has been as unresponsive to medication as any level below it. Otherwise, I'd of been in the ER in a heartbeat.
- Interventional procedures: In my last post, I mentioned that I'd be starting a few rounds of cervical epidurals with Dr. O'Connor at AZ Innovative Pain. This is an injection of a steroidal anti-inflammatory under x-ray guided fluoroscopy into the epidural space that surrounds the nerves at the junction of C7-T1, which then disperses throughout the cervical spine. The initial plan was to do three of these, a few weeks apart. But after zero response to the first two, we decided a third wasn't warranted. So where the heck to go from here? After chatting with Dr. O'Connor last week, we decided to pivot in a different direction: occipital nerve blocks.
If those sound familiar, it's because I've had occipital nerve blocks before (quite a few times actually). In all these years, the only real substantial relief I've ever had (from a diagnostic or therapeutic procedure) was the occipital nerve blocks with Dr. Peled in San Francisco, which confirmed my candidacy for my first occipital nerve surgery in 2017. Granted, I didn't get relief from the surgery itself, a decompression of my left and right greater occipital nerves, decompression of my right and left lesser occipital nerves, and excision of my right and left third occipital nerves. We have no idea why that surgery, and the next one just a few months later - excision of my left lesser occipital nerve - didn't provide lasting relief. All I know is what I felt after the preoperative diagnostic blocks. And out of sheer desperation today, that's what I'm chasing...because what choice do I really have? So I'll head back to the surgery center tomorrow for my first round of ON blocks. We'll see how I respond and go from there.
Dr. O'Connor also just referred me to a local neurosurgeon for a second (or 132nd?) opinion. Given the nature of and complexity of my case, and given that I haven't seen a neurosurgeon since my neurosurgery in FL in 2015, we all agreed this would be a valuable step. I should be seeing Dr. Abdulhamid at Royal Spine Surgery soon.
- CrowdMed: Earlier this winter, I submitted my case, in all of its exhaustive detail, to CrowdMed. Crowdmed is basically a crowdsourcing tool for complex medical conditions. As the patient, you answer questionnaires that cover your personal story, medical history, current symptoms, etc. and medical detectives with a broad range of expertise can weigh in. One physician agreed that there was likely a central sensitization component to my pain at play (which is probably accurate) but that was really the extent of takeaways. Even though it didn't amount to a whole lot for me, I wanted to share it here because I do think there's a lot of merit to the concept. If you're suffering like me and would do anything for help, you've got to cast as wide a net as possible.
- Brr. Cold water immersion is something I've done periodically over the years, but never on a super consistent or regimented basis. I'd hop in the cold plunge at EXOS after a workout (prior to getting pregnant) or do some contrast therapy here and there, but over the last few months, I've gotten into a solid routine here at home. Why do I put myself through this, you might be wondering? Simply put, cold water immersion is regulation training. You're trying to improve the flexibility of your autonomic nervous system, which is really useful for people who spend the majority of their day in sympathetic-dominant scenarios (chronic pain!). By submerging your body in frigid temperatures, you induce a fight or flight response and your body is forced to react against it. Your breathing normalizes over time (fairly automatically, believe it or not) and it gets easier and easier each time you take the plunge.
Through the winter, I was able to get away with using our pool, which stays in the high 30s to mid 40s, but as the season shifting and the pool's warming up, I've moved to the homemade cold plunge Craig had installed a few years ago. I go in for just two minutes every morning (you can do anything for two minutes). I'm a super early riser - up by 4:10, workout done by 5:15, out of the moon-lit cold plunge and into the shower by 5:20. I know it seems nuts to a lot of people, but when I wake up each morning already engulfed in pain that gnaws at my body and brain with every passing hour of the day, this routine is my way of taking control. I might feel knocked down again and again, but I need to at least start standing up.
It'd be a big stretch to say the cold provides pain relief, but some days I do feel like it can give me a little extra breathing room.
- Neurology check-in: At the end of the year, Craig and I hopped on a phone call with my long-time neurologist from the Mayo Clinic, Dr. Dodick. Even though I haven't had any real success with some of the more conventional migraine protocols, we're grateful to have had Dr. Dodick in our corner through the years. He's one of the leading headache and migraine researchers in the world, on the bleeding edge of innovation that is shaping the landscape of migraine treatment. I know this is the case in many other areas of medicine too, but I find it quite remarkable how many treatment options have emerged just in the last eight years I've been under his care.
From the noninvasive wearable or handheld modalities I've tried like the Cefaly, vagal nerve stimulator, and transcranial magnetic stimulator, to calcitonin gene-related peptide (CGRP)-blocking antibodies, the technology has come so far. And when you live in unresponsive chronic pain like I do, constantly toeing the line between utter hopelessness and cautious optimism, that's the stuff that gives you real, tangible hope. Because Dr. Dodick is on the frontline of this research, helping to get these treatments FDA-approved and accessible to patients like me, he's been able to share updates with me and Craig in real time too. Anecdotal information like "this device is so far just approved for the use of cluster headaches ... BUT we've been seeing that it's also helping chronic daily headache so it might be worth it for you to try..." (as an example).
So a few interesting takeaways shared on this recent call:
We chatted with Dr. Dodick about the vestibular component of my pain. "Dizziness" has never been a primary complaint for me (I'm lucky that I don't deal with debilitating vertigo, as that is a beast on its own. But, as discussed in my last post (and the reason I was trying the Z Health rehab), there is obviously a reason I get dizzy when turning my head left to right more than two or three times. He agreed this stems from my original injury. Hitting that tree was a vestibular insult, leaving my system highly vulnerable to equilibrium changes. It therefore makes perfect sense that changes in visual input (via the vestibulo ocular pathway) and input from the neck (via the vestibulospinal tract pathway) can still have a profound effect on my symptoms.
We asked Dr. Dodick what he thought of the red spots that sometimes develop on particular "spiked" pain days. (See photo below). His take was that the blotchiness was likely indicative of reflex sympathetic dystrophy, or more commonly referred to as complex regional pain syndrome (CRPS). Basically, this is autonomic nervous dysfunction (no surprise there). When you sustain an injury, your sympathetic nervous system tells your blood vessels to constrict to prevent blood loss and then later, to open back up so that the damaged tissue can be repaired. But with CRPS, your poor sympathetic nervous system gets mixed signals. Even though the injury is over and done with, that message is never received. It's the reason why amputees can experience phantom limb pain. It's almost unbelievable, but it's a horribly real thing. (Pain happens in your BRAIN, so you can still feel pain in your left leg even if you've lost your left leg). CRPS is treated with pain relievers, anti-inflammatories, anti-depressants, steroidal injections, even intravenous ketamine infusions. And those are all things I've already done, so it doesn't really change a whole lot for me. Just interesting.
On the modality front, Dr. Dodick recommended I try a new remote electrical neuromodulation device called Nerivio, which recently gained FDA approval for the acute treatment of episodic or chronic migraine. My pain is 24-7, which makes it hard to treat in acute manner (think taking an abortive drug when you feel a migraine "coming on") but Dr. Dodick thought (and we agreed) that it couldn't hurt to try. The Nerivio works by engaging a descending pain inhibition network in the body. It's just an arm band that feels kind of like a tens unit and you control the intensity from an app on your phone. So I gave that a shot but didn't experience any relief.
We revisited a conversation we've been having over the last couple of years around calcitonin gene-related peptide (CGRP)-blocking antibodies too. As I mentioned before, these therapies are already considered transformative in this field of medicine, and it's early days still. Monoclonol antibodies are designed to target a single protein or receptor that's responsible for transmitting pain signals during a migraine. When they enter into the body, they break down into their amino acids. Unlike other drugs, they don't get metabolized by the liver, they don't attach to other proteins, and they don't target other stuff along the way, which means that the side effects (especially compared to traditional migraine meds) are so minimal.
If you've been here for a while, you know I'm not your run of the mill migraine migraine patient, so as exciting as some of these breakthroughs are, they don't always mean a whole lot for me. But Dr. Dodick explained that CGRP trials are now underway for acute, subacute, and chronic post-traumatic headache (hey that is me!). The only reason we haven't gone down this path before is that in the time since they've gained approval and come to market, I've been undergoing fertility treatment, and then have been pregnant, and am now still breastfeeding - all of which are contraindicated. As soon as that's not the case, I'll most certainly be starting. Dr. Dodick has recommended an IV version, as bioavailability is 100% whereas the self-administered monthly shots are only about 50%.
We also discussed some additional research he's been doing with post-concussion syndrome. He recommended I try supplementing with N-acetylcysteine (NAC) ( 600mg 1-2/day), which I've been on now for a couple of months. NAC is a precursor molecule to our body's main antioxidant, glutathione. It's been studied in traumatic brain injury patients for its neuroprotective and mitrochondrial boosting benefits.
Along the same lines, we talked about the potential therapeutic benefit of nictotinamide riboside, a precursor to NAD+. If you're not familiar, NAD+ (which stands for nicotinamide adenine dinucleotide) is a coenzyme of vitamin B3 (niacin). It's naturally present in every cell in your body and its main role is the transfer of electrons from one molecule to another. Simply put, it's what FUELS metabolic reactions, driving your cells to metabolize carbohydrates, fats, and amino acids for energy. Thorne makes a product called ReveraCel that combines nictotinamide riboside with a few other things so he recommended I try that too (which I also have been now for a couple of months).
It's clearly advantageous to boost NAD+ (Dr. Dodick is even working with Thorne to develop a product containing both nictotinamide riboside and NAD to help treat post-concussion syndrome) so we asked about NAD+ infusions. NAD+ is currently used therapeutically to treat a host of different age-related, inflammatory, autoimmune, and neurologic conditions. It's even used in addiction recovery because of its ability to aid in the regeneration of opiate receptors, which is pretty fascinating. It's most beneficial when administered intravenously, sending a high dose of the compound directly into the bloodstream. He wasn't aware of any research with this kind of chronic pain, specifically, but agreed it wouldn't hurt for me to try. If mitochondria make energy and NAD+ can optimize the function of my mitochondria, seems worthwhile in my book. So I'll be going to my naturopath for my first 90 minute infusion on Thursday. The plan is to do at least three.
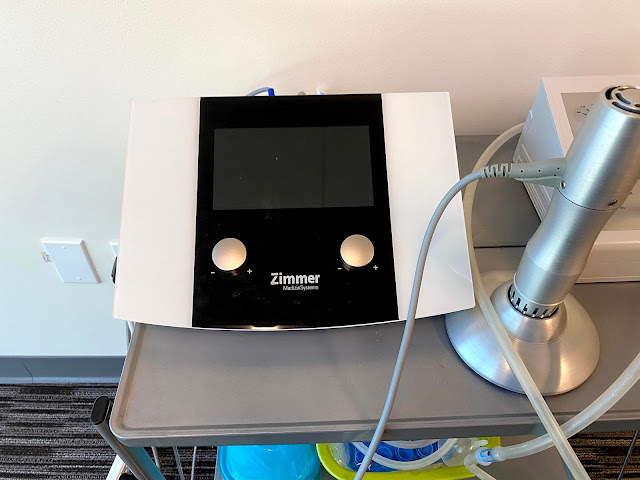
- Shockwave Therapy
As time has gone on, it can feel increasingly difficult for me to start working with new practitioners. It's overwhelming to start from square one, and honestly just hard for me to even find clinicians who offer something more or different than what I've already tried over and over and over again, But when I was referred by a friend and highly respected expert in the field to Shawn Robeck, DC at Fix Body Group I knew it was worth a fair shot. We started working together with a focus on just restoring some function back to my cervical spine. Along with manual work and a few other modalities I've been treated with in the past (like ARP wave and traction), he started using a tool that was new to me: Shockwave. This is what the unit looks like below. It's essentially a wand that uses a mechanical pressure wave, which is transferred to the body by an applicator head and which radiates outs in the tissue. That mechanical stress triggers reactions in the tissue that should promote healing. If you're familiar with the mechanism of prolotherapy or platelet-rich plasma therapy, it's very similar. You create trauma in a specific area to force the the body into healing. Shockwave therapy is NOT comfortable, especially in certain areas like the ridge between my occipital and parietal bones, where we've focused on breaking up adhesions. It kind of feels like someone is drilling into your skull. But it's also a good kind of pain, as only someone in chronic pain can understand.
In the first few weeks working with Shawn, it seemed like I was actually experiencing some shifts in my pain, along with improved mobility in my c-spine. In fact, I even had a week in late January (and ENTIRE WEEK) of lower-than-normal head pain. It may not seem significant, but that was f-ing remarkable. That relief has been difficult to replicate, which is incredibly frustrating, but we're keeping at it for now.
- Red Light Therapy
One of the perks of Craig's career is that he himself is highly knowledgeable in a lot of these less conventional therapies, or well connected to those who are. So recently we were connected with a company called LightStim, whose products combine therapeutic light energy with patented technology to aid in the body's natural recovery process. In the same way that plants absorb light energy from the sun, these devices deliver different wavelengths of light energy to help increase local blood circulation and relieve pain. We have this bed at our house right now, which I'm trying for a couple of months. I go on it every day for 40 minutes (20 front and 20 back). I haven't noticed any changes as of yet, but will report back.
Phew. That was a lot, but I think that about covers it for now. I try so hard to stay positive. It's easier said than done but I know that ultimately, the quality of my own life will depend as much on how hopeful I chose to be as it does a number on the pain scale.
I was listening recently to some parenting podcast all about teaching kids resilience skills. "Resilience" is kind of one of those buzzwords that gets tossed around, but there was this one line about what it is and what it isn't that struck me. Basically that resilience isn't the ability to persevere through challenge but the ability to take stress and pain and to use it to your advantage; to grow from it in a purposeful way. They talked about how resilient people are good at finding pause to problem solve. This was all in the context of raising good humans, of course, but at the very least, this will be what Ryan can learn from her mama. (I can only hope that my chronic pain lens will help me be a better parent as much as being a parent has helped me live in chronic pain).






Hi and thanks for keeping up the blog. I've followed you for a while since I suffer from the same problem, with similar mechanism of injury. One thing that I think to keep in mind is that your neck has suffered an important trauma (as well as invasive procedures) and could have weakened muscles. Combined with lengthy computer work (especially on a laptop, if looking down) or changes to posture of the upper spine,this can stress the upper back and neck which refers pain through the occipital nerves and gives you a "headache" or "migraine". In fact, these nerves are on the skull, just below the scalp. With a whiplash type of injury, you often have to rehabilitate the neck to get rid of headache and pain behind the eye, symptoms of Arnold's neuralgia. Neck stretching and strengthening takes months, but it gave me some relief. Best wishes, Marc.
ReplyDeletehttps://bitmainantminerforsale.com
ReplyDelete