So I'll pick up where I left off in November. I was preparing to head back to San Francisco in mid December for Dr. Peled to cut my third occipital nerve, which had been decompressed back in July but was showing obvious signs of lingering damage.
I had a few other procedures scheduled here in Arizona prior to surgery, though. First, was more Botox. This was my third round in six months, and I can't say I was super optimistic going into this one, given that I hadn't felt any improvement until then (coupled with the fact that I didn't have a positive outcome the first time I tried it close to four years ago either) BUT, my Mayo neurologist and his PA had reminded me that for some of their patients, it really does take multiple rounds for the Botox to make a dent. On some of the online occipital neuralgia support groups and forums that I belong to, I often see people talk about how painful these injections are for their migraine treatment (or how much they dread or fear procedures like this). Maybe it's a testament to how many times my head and neck have been poked and sliced into, or maybe I'm just a complete wacko, but there's something about the feeling of a half inch needle going into my sore head that actually feels good. Almost like a massage therapist digging into just the right spot. Unfortunately, that feeling leaves with the needle.
Here's a breakdown of the Botox injection sites:
5 units in the procerus
5 units in 2 injection sites in the corrugators
20 units in 4 injection sites across the frontalis
20 units in 4 injection sites in the right temporalis
20 units in 4 injection sites in the left temporalis
25 units in 5 injection sites in bilateral parietal region
20 units in 2 injection sites in bilateral masseter muscles
15 units in 3 injection site to the right occipitalis
20 units in 4 injection sites in the left occipitalis
20 units in 4 injection sites in bilateral cervical paraspinal muscles
30 units divided evenly across a total of 6 injection sites in trapezius muscles
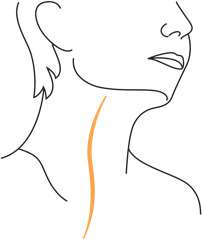
In early December, I went back to Mayo for bilateral auriculotemporal nerve blocks and a series of trigger point injections. You can see the location of the auriculotermporal nerve below. The area over bilateral temporoauricular nerves was injected with 2.0 mL of 0.5% Bupivacaine. 0.5 mL was injected 2 cm anterior to each tragus bilaterally. An addiontal 0.5 mL was injected into each of two tender spots in the temporal region which followed the nerve distribution bilaterally. As a side note, this is the only nerve block procedure I've ever had (and I've had a lot) that has left lasting tenderness at two of the injection sites near each temple. Weird.
And here's a breakdown of my trigger point injections:
The area over 12 trigger points were identified in bilateral cervical paraspinal and trapezius muscles, followed by a 30-gauge 1/2-inch needle 0.5% bupivacaine. 0.5 mL of 0.5% bupivacaine was injected into each of 12 identified trigger points.
Then, just a few days later, it was time for Craig and I to fly back to San Francisco for surgery. Dr. Peled's office is in the city, but this time we opted to stay in the east bay where the surgery center is. We knew we'd rather spend any downtime getting some fresh air in Walnut Creek. If surgery-eve sunset hikes are your thing (no? just me?), Acalanes Ridge is where it's at.
On December 11, we reported to the surgery center first thing in the morning. (Thank God, because meal skipping is not my strength.)
This procedure didn't take quite as long as the one in July because instead of having four nerves decompressed (right and left greater occipital nerves and right and left lesser occipital nerves) and having two excised (right and left third occipital nerves), I was only having my left lesser occipital nerve excised. Since I was under for less time, I also had a much easier time waking up from anesthesia this go around.
Like my first surgery, I woke up feeling surprisingly good. Drowsy, but perfectly capable of walking into Whole Foods and eating most of the prepared foods bar on our way back to the hotel. I spent the rest of the afternoon just resting with ice packs in rotation (wrapped up to keep my incision dry). I had filled the prescriptions for the pain killers that Dr. Peled had written (and then forgot them at home...and then had them refilled in CA) but just like last time, I really didn't have enough discomfort to warrant taking them. I did stay on a regular dose of CBD oil (not sure how much, if any, it helped) Then I rested the majority of the next day, but even went for some short walks in town (lying stiff in bed always feel so uncomfortable to me).
On Wednesday morning, Craig and I met with Dr. Peled for a follow-up before flying home. You can see here what my incision looked like (day 3) as he removed the bandage to change out the steri strips.
For the first few weeks after surgery, numbness around my incision and throughout the lower portion of my scalp and behind my ear was at an all time high (which, truthfully, doesn't both me at all) and pain throughout my head was at an all time low. Then, the "honeymoon period" ended and I started having increased pain along the top, frontal, temporal, and supraorbital regions of my noggin. But I knew from my first surgery that this wasn't an uncommon occurrence. When nerves are decompressed or cut, part of the recovery process often involves other nerves becoming hypersensitive in response. Kind of a "what the hell is going on back there?" reaction. That made for some tough days (which, I can't really say are over just yet) but the most important thing was that the area around my lesser occipital nerve was ..and still IS...feeling good. That in itself is my greatest source of optimism, especially given that those other regions of my head did calm down with the pre-operative diagnostic block to that nerve. In other words, I have good reason to believe that in time, everything else should start feeling better.
The steri strips fell off about two weeks later, and here's what this beautiful neck of mine looked like then. Still some inflammation around the incision, but not bad.
Over the last month, the theme for me has been patience. Of course that doesn't mean I've felt patient or acted patient (sorry, Craig) but I know this recovery just takes time.
A few weeks ago, I had a follow up with my neurologist, Dr Dodick. It's been an interesting experience navigating this occipital neuralgia diagnosis and occipital nerve surgeries without the full support or participation of my neurology team. I understand the need for more research and more data supporting the efficacy of this treatment, but it's frustrating to realize how little collaboration there is. Peripheral nerve surgery is obviously not the solution for every migraine patient. But I mean, shit, there are A LOT of people whose lives it is saving (yes, saving)...people like me who have exhausted virtually every other conventional and alternative treatment and are left with very few answers and very little hope. Isn't that at least worth paying attention to?
Anyway, Dr. Dodick advised against continuing with a fourth round of Botox (something we had previously discussed) and against retrying a newer model of the Cefaly device, the Cefaly Dual (something I had talked about how his PA back in November). I first tried the Cefaly back in spring of 2013 without success. This device attaches to your forehead and generates very precise electrical impulses to stimulate the nerve fibers selectively. Dr. Dodick explained that he's actually had some chronic daily headache patients get worse on the Cefaly and then not rebound back. What a treat that must be.
Pretty confident that it wouldn't make things any worse, he did want me to try the gammaCore non-invasive vagal nerve stimulator a shot though. Currently, the gammaCore is only FDA-approved for cluster headaches but it will be approved later this year for migraines and he's had some anecdotal success using it with patients of various headache disorders. So although no yet covered by insurance (AKA not cheap), we figured it was worth a shot.
gammaCore activates pain-relieving power through non-invasive vagus nerve stimulation
gammaCore (nVNS) activates your vagus nerve with a patented, gentle electrical stimulation, providing relief from cluster headache pain in a very different way than drugs.1
- The vagus nerve is an important highway of communication between your brain and many parts of the body2
- The vagus nerve plays an important role in regulating pain2
Non-invasive vagus nerve stimulation with gammaCore is believed to help block the pain signals that cause cluster attacks.2,3
- Unlike traditional vagus nerve stimulation therapies, gammaCore stimulates the nerve non-invasively through the skin1
- Avoids many drug-like side effects and the injecting, inhaling, or ingesting associated with medications1
- gammaCore is FDA-cleared and has been used in Canada and Europe for several years4
The gammaCore is supposed to be something you use for at least a month (sometimes more) before really knowing if it's helping, but it became very clear after a few days using it that I wasn't responding well. I had some MAJOR flares in my frontal pain, which seem to subside when I'd been off it it for a week or so. So that's done with.
So right now, at the six week mark, I'm slowly start easing back into my regular workouts ("take off like an airplane, not a rocket" as Craig said yesterday morning before I practically skipped out the door at 5:30 am to the gym). In physical therapy (and on my own), I'm also working to improve some of the issues I have going on down the chain. I have so much neural tension through my left shoulder and arm that in order to allow for movement of my head, my left levator scapulae becomes over active. As a result, my long thoracic nerve is irritated. Layered on top of my head pain, all of these issues seem overwhelming (at least to me) but ultimately, I know it's all connected (whether to my original injury or just a product of all of the trauma my body's been through in the last 6.5 years. The lower I can get my head pain, the more manageable everything else seems. Like all of life actually.
Aside from the infrared sauna (which I try to get in daily), I've started getting back in the cold plunge regularly. Cold immersion (including contrast with hot), especially when preceded by short interval sprints (:20 on the bike with pretty high resistance) just seems to give me some better days. I'm not sure if it's a hormonal response or what but I'll take it.
I also just started taking these Charlotte's Web capsules from CW Simply. I've used Charlotte's Web in oil form before but through a work introduction, Craig recently spoke to a neuroscientist whose primary research focus is using cannabis to treat pain and in his experience, he's found these tablets to be most effective as compared to the various other forms. So, I'm only on day #2 but I'll keep you posted as to whether it seems to help.
Lastly, I came across this blog post a few weeks ago...written by another CA-based plastic surgeon who performs the same procedures I've had with Dr. Peled. It's titled "Head Trauma, Whiplash, and Migraine Headaches" and it caught my attention for obvious reasons. Since I know that many of the people who land on my blog are dealing with chronic head pain for the very same reasons, I thought it was worth sharing. Dr. Lowenstein provides an excellent explanation of exactly how occipital neuralgia can develop in patients like us. There aren't words to describe just how difficult it is to live with this kind of pain (some of us, for so long) yet still not understand or be be able to explain what exactly is even causing it.
Thanks to Dr. Peled, I now have understanding, validation, and (almost...I'm getting there) resolution of mine.
Here's an excerpt below, but it's worth the whole read.
"...in many cases, it is the second part of the head trauma, the neck whiplash that can be the culprit in ongoing, chronic, or recurring migraines and head pain. Imagine what happens to the muscles of the neck when head trauma is imminent… the neck’s role in the human body is to keep the head stable. When there is unusual motion or the body senses that there is about to be trauma to the head, the neck’s role is to tense up and try to prevent the head from hitting anything, and if it has his something, the neck is supposed to prevent the head from bouncing back or hitting something again.
In these cases, the main stabilizing muscles of the neck become tense and strong and try to keep everything safe. The forces of the heavy skull and brain moving in one direction while the neck is working hard to stabilize things is what creates the whiplash injury. Duriare this situation, the tissue of the muscles- both the muscle cells themselves as well as the fascia, or connective tissue, in and around the muscles can become damaged. This damage can come in the form of micro-stretches or even tears of the muscles or fascia tissues.
The occipital nerves run through the muscles of the neck. From the level of the spine, the nerves course through and around several muscles including the splenius capitus, the trapezius, and the sternocleidomastoid muscles. All of these muscles tense up in order to stabilize the head in cases of trauma. Tightening of these muscles around the nerves is a common circumstance in head trauma, and anyone who has experienced head trauma can describe the sore muscles associated with the days or weeks following the event. What is actually happening is the same kind of thing we see when we “pull” a muscle- stretching and tearing of the muscles tissue creates soreness, and the muscle is then repaired in time, often with some degree of scar tissue.
Athletes who experience “pulled” muscles often go through physical therapy and massage. These therapies are meant to re-stretch the muscle tissue and loosen up scar tissue. But do patients who have a history of “head trauma” go through the same muscle care? Sometimes, but not often, and not often early enough to prevent chronic scarring. The neck tissue that is stretched and torn heals with scar tissue and often creates the permanently tight tissue that can compress the nerves going through it. Tight muscles and fascia, often associated with scar tissue and even chronic inflammation, cause compression to the occipital nerves in both the short and long-term after these head traumas. Studies have shown that this nerve compression can often be the triggering signal that sends a distress call to the brain, triggering head pain and migraine headaches.
It is no surprise that we often see that patients with a history of head trauma have migraine headaches develop either immediately or shortly after their injury. While a subset of these patients has primary brain issues that cause short and long-term head pain, many of these patients actually have a condition that is correctable by migraine surgery."










Thank you for sharing your story. I too met with Dr. Peled. I would love to hear how things are going for you now when you get the chance to post again. Wishing you well and all the best!
ReplyDeleteThanks for sharing your experience.
ReplyDeletegood posture brace
I had the nerve ablation on both sides, and was very hopeful because it gave me 30 blissful days of no pain, but I am now back where I started. I've had ON since 2010 with migraines 3-4 times a week. Seeing my chiropractor again out of desperation. I would love to hear the results of your surgery. I'm having trouble finding anyone who has found treatments that have worked for longer than a few months.
ReplyDeleteCould you please tell me the contact of neck movement trainer so that i can also gain my neck movement
ReplyDeletehttps://bitmainantminerforsale.com
ReplyDelete